|
Milton J.
Stern, DPM
What is a Bunion?
 A
bunion is an enlargement of the bone at the base of the big toe. The
medical term for this condition is Hallux Valgus, which means a
turning outward of the great toe. Bunions are one of the most common
forefoot deformities. These usually begin when the big toe starts
moving toward the smaller toes because of the shoe gear. This
shifting of the bones causes a bony prominence on the side of the
patient’s foot (the bunion joint). Over a period of time the big toe
may come to rest under (occasionally over) the 2nd toe. A bunion is
more common in women then men due to the fact that women tend to
wear tighter shoes. Wearing high heel shoes even further puts stress
on the bunion because all the body’s weight rests there.This
condition can cause a variety of different soft tissue and bone
complaints, which may result in severe pain. A
bunion is an enlargement of the bone at the base of the big toe. The
medical term for this condition is Hallux Valgus, which means a
turning outward of the great toe. Bunions are one of the most common
forefoot deformities. These usually begin when the big toe starts
moving toward the smaller toes because of the shoe gear. This
shifting of the bones causes a bony prominence on the side of the
patient’s foot (the bunion joint). Over a period of time the big toe
may come to rest under (occasionally over) the 2nd toe. A bunion is
more common in women then men due to the fact that women tend to
wear tighter shoes. Wearing high heel shoes even further puts stress
on the bunion because all the body’s weight rests there.This
condition can cause a variety of different soft tissue and bone
complaints, which may result in severe pain.
What causes a Bunion?
There is no one single cause of
bunions. A bunion is commonly a symptom of faulty mechanics of the
foot. The
 imbalance
of the forces on the big toe causes the bunion deformity to start
and increase progressively with time. Usually there is abnormal foot
function, with excessive pronation. This is the excessive rolling in
of the foot at the ankle joint while you are walking. The deformity
seems to run in families so there is an inherited component. Those
people with flat feet seem to develop the typical bunion whereas
people with high arches develop the arthritic type bunion more
frequently. No matter what type of foot you have inherited it is the
type of shoes that make the progression of the bunion increase. The
most important causative factor is poor fitting footwear. This
accounts for a higher incidence among women than men. As the big toe
is pushed toward the second toe by our shoes, it changes the
structure of the joint. The skin and deeper tissues deform, become
inflamed and swell. Some systemic problems such as rheumatoid or
osteoarthritis can cause bunion development of bunions. If one leg
is longer that the other then the longer leg is more inclined to
develop a bunion. Trauma to the first joint can set an arthritic
type bunion. People with very flexible feet tend to develop bunions. imbalance
of the forces on the big toe causes the bunion deformity to start
and increase progressively with time. Usually there is abnormal foot
function, with excessive pronation. This is the excessive rolling in
of the foot at the ankle joint while you are walking. The deformity
seems to run in families so there is an inherited component. Those
people with flat feet seem to develop the typical bunion whereas
people with high arches develop the arthritic type bunion more
frequently. No matter what type of foot you have inherited it is the
type of shoes that make the progression of the bunion increase. The
most important causative factor is poor fitting footwear. This
accounts for a higher incidence among women than men. As the big toe
is pushed toward the second toe by our shoes, it changes the
structure of the joint. The skin and deeper tissues deform, become
inflamed and swell. Some systemic problems such as rheumatoid or
osteoarthritis can cause bunion development of bunions. If one leg
is longer that the other then the longer leg is more inclined to
develop a bunion. Trauma to the first joint can set an arthritic
type bunion. People with very flexible feet tend to develop bunions.
What are the symptoms of a Bunion?
 The
patient’s feet may become too wide to fit into their normal size
shoe. Redness, swelling and pain may be present along the inside
margin of the foot. Moderate to severe discomfort may occur when the
patient is wearing tight shoes. A hammertoe may occur of the 2nd
toe. This is when the toe contracts and allows the toe to press on
the shoe. Subsequently, this may cause a corn on top of the second
toe. A painful callus may develop over the bunion or at the bottom
of the foot. A callus usually occurs on the sole of the foot
directly under the second toe. Painful corns may develop due to
abnormal pressures being exerted on to the foot. These may occur in
between the 1st and 2nd toes and on the 5th toe. There may be
irritation caused by the overlapping of the 1st and 2nd toes.
Stiffness may occur at the big toe due to secondary arthritis
occurring, this is known as hallux rigidus. The bunion may have a
fluid filled sack called a bursitis. This can be very painful and
can become infected. An in growing toenail may occur on the 1st toe
due the excessive pressures being applied to it. In some cases, due
to the chronic pressure caused by the bunions, the corns, calluses
or bursitis present can become ulcerated and infected. The
patient’s feet may become too wide to fit into their normal size
shoe. Redness, swelling and pain may be present along the inside
margin of the foot. Moderate to severe discomfort may occur when the
patient is wearing tight shoes. A hammertoe may occur of the 2nd
toe. This is when the toe contracts and allows the toe to press on
the shoe. Subsequently, this may cause a corn on top of the second
toe. A painful callus may develop over the bunion or at the bottom
of the foot. A callus usually occurs on the sole of the foot
directly under the second toe. Painful corns may develop due to
abnormal pressures being exerted on to the foot. These may occur in
between the 1st and 2nd toes and on the 5th toe. There may be
irritation caused by the overlapping of the 1st and 2nd toes.
Stiffness may occur at the big toe due to secondary arthritis
occurring, this is known as hallux rigidus. The bunion may have a
fluid filled sack called a bursitis. This can be very painful and
can become infected. An in growing toenail may occur on the 1st toe
due the excessive pressures being applied to it. In some cases, due
to the chronic pressure caused by the bunions, the corns, calluses
or bursitis present can become ulcerated and infected.
What can you do for a Bunion?
Wear wide fitting shoes, preferably with a leather
upper, which will allow a stretch. Make sure the shoe has a good
support structure, which will control foot motion. Use an arch
support also to control abnormal foot motion. Avoid high-heeled
shoes. If your bunion becomes painful, red and swollen, try using
ice on the joint and elevate the foot on a stool. Apply a commercial
bunion pad, making sure it is not too rigid or medicated. A bunion
shield can reduce the pain over the bunion. Apply a moisturizer
twice daily to hard skin and use a pumice stone to reduce the
thickness of the hard skin. Ignoring the condition hoping that it
will go away on its own is not a good idea. Do not try to remove any
painful build up of skin yourself. This includes picking at them or
using a sharp razor blade to remove them (especially if you are
diabetic).
What the podiatrist will do for a Bunion?
With most orthopedic conditions in the
foot there are several different treatment plans available. The most
important first line treatment is to adequately diagnose the
condition. Once the condition is diagnosed there are usually three
different approaches. The first is to do no active treatment but
just to monitor the condition.
Have the patient follow the above steps in “What you can do for your
bunion?” The second option is to accommodate the foot. By this we
mean treat the pain. This might include injections, strapping of the
foot, arch supports, physical therapy or oral medications. When we
accommodate we don’t make the deformity go away, but try to make the
pain decrease. The third option is to correct the condition. For
bunions this always requires some sort of surgical intervention.
There are two main reasons to consider surgery for your bunions. The
first is if you are in pain and conservative care has not rendered
you pain free. The second is if you have a deformity that
progressively has gotten worse and waiting would require more
extensive surgery at a later date.
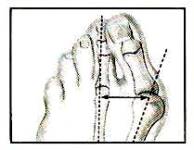 Evaluation
of the bunion is essential to the proper surgical approach. The most
important consideration is the angle between the first and second
metatarsal.This is called the IM angle.This stands for the
inter-metatarsal angle. The picture on the right shows that angle.
We have three different surgical approaches based on this angle. Of
course the structure of the rest of your foot also adds to our
decision. If your IM angle is 0-10 degrees we call this a simple
bunion. We can just remove the bunion bump and do some soft tissue
work around the bunion. Usually you can walk on this the same day as
the surgery. Evaluation
of the bunion is essential to the proper surgical approach. The most
important consideration is the angle between the first and second
metatarsal.This is called the IM angle.This stands for the
inter-metatarsal angle. The picture on the right shows that angle.
We have three different surgical approaches based on this angle. Of
course the structure of the rest of your foot also adds to our
decision. If your IM angle is 0-10 degrees we call this a simple
bunion. We can just remove the bunion bump and do some soft tissue
work around the bunion. Usually you can walk on this the same day as
the surgery.
If your IM angle measures 11-14 degrees
we call this a moderate bunion. If you just take off the bump as a
simple bunion then the chances of the bunion reoccurring increases.
We want to try to decrease this angle. We try to move the metatarsal
head closer to the
 second
metatarsal. This effectively reduces the IM angle by up to 4
degrees. There are sometimes additional corrections needed to
straighten the big toe. By moving the head of the metatarsal over in
a moderate bunion the recurrence rate goes down drastically. Usually
this requires you not to walk on the foot for a period of 10-21
days. second
metatarsal. This effectively reduces the IM angle by up to 4
degrees. There are sometimes additional corrections needed to
straighten the big toe. By moving the head of the metatarsal over in
a moderate bunion the recurrence rate goes down drastically. Usually
this requires you not to walk on the foot for a period of 10-21
days.
If your IM angle is over 14 degrees we call this a
severe bunion. This usually requires work to be done at the base of
the metatarsal. We can reduce the IM angle to almost zero depending
on the structure of the rest of the forefoot.This requires you not
to walk on the foot for a period of 6-7 weeks. A combination of
procedures may be necessary with severe bunions. We may need to do
work at the head of the bunion also.
 With
all these bunions we evaluate how much the big toe is drifting
towards the second toe and we also evaluate the joint itself. Each
of these may require a little extra work. If the joint is totally
arthritic and cannot be saved then it might have to be replaced with
an artificial one. Many of the arthritic joints if caught early
enough can be saved or at least not need artificial joints for a
more prolonged period of time. With
all these bunions we evaluate how much the big toe is drifting
towards the second toe and we also evaluate the joint itself. Each
of these may require a little extra work. If the joint is totally
arthritic and cannot be saved then it might have to be replaced with
an artificial one. Many of the arthritic joints if caught early
enough can be saved or at least not need artificial joints for a
more prolonged period of time.
Bunion surgery has come along way over the last 30
years and the recurrence rate had dropped dramatically as long as
you properly evaluate the IM angle on the weight bearing x-ray. |